|
intra-peritoneal what? ex? |
|
Stomach, First part of the duodenum [5 cm], jejunum, ileum, Cecum, appendix, structures completely surrounded by visceral peritoneum transverse colon, sigmoid colon, Rectum, Spleen, Uterus, Fallopian tubes, ovaries |
|
retroperitoneal (primary) what examples |
|
structures that develop behind the peritoneum and stay there kidneys, ureters, suprarenal glands, aorta, IVC, post wall o nerves, nerve plexuses |
|
retroperitoneal (secondary) what? ex? |
|
structures who develop interperitoneally but end up fusing (partial/whole) to the posterior abdominal wall 3/4 duodenum, ascending/descending colon, pancreas |
|
kidneys location (vert) which one higher? |
|
- lie on posterior aspect of abdominal wall, T12 - L3. Behind peritoneum - upper kidney protected by two floating ribs -right kidney lower than left. liver pushes it down (a few inches) |
|
layers of kidney inside to outside |
|
renal medulla renal cortex renal capsule (tough fibrous) perinephric fat (or "perirenal fat") renal fascia paranephric fat (or "pararenal fat") peritoneum (anteriorly), and transversalis fascia (posteriorly). |
|
Hilum of kidney points in what direction what's there, what orientation? |
|
points medially renal artery/vein and renal pelvis VEIN MOST ANTERIOR, THEN artery then pelvis |
| quick kidney function run though |
|
cortex (nephrons) - medulla, collecting duct pyramids - apex of pyramid/ renal papilla - minor calyx - major calyx - renal pelvis - ureter
cortex has nephrons/tubules medulla has collecting ducts (renal pyramids)
|
| when renal artery reaches hilum it branches into how many segments? |
|
5 END ARTERIES superior, anterosuperior, anteroinferior, inferior and posterio |
|
variation of renal arteries why? in what % of people what should end up with |
|
should have 1 renal artery/kidney. they ascend from pelvis and continuously re-establish/lose blood supply as they go. failure of fetal blood supply to degenerate results in accessory vessels. |
|
hydronephrosis what is what caused looks like? |
|
distention/dilation of renal pelvis caused by obstructed urine flow. large bags in pelvis can be caused by accessory renal artery that hardens/compresses the ureter |
|
three anatomical narrowing sites of ureter what gets lodged? |
|
urtero-pelvic junction (ureter - pelv) mid ureter (where iliac art crosses) utero-vesicle junction (ureter-bladd) kidney stones (calculi) |
|
symptom of kidney stone where? |
|
severe pain in scrotum in spinal cord segments that innervate T11-L2 lumbar to groin |
|
treatment of kidney stones surgical? special precaution another? |
|
surgically enter posterior lithotripsy (focused shockwave) |
|
Embryological development of kidney -from where? -what happens? - from what embryonic layer? - gland growth? - what's fetal kidney look like? |
|
from pelvis ascend and rotate so ureters face medially mesoderm adrenal glands originally as big as kidney and shrink as kidney grows fetal kid is lobulated |
|
fusion misformations types (2) |
|
horseshoe (fusing at pelvic brim) sigmoid (S shaped) |
|
horseshoe kidney -ascend until where? -orientaton of ureters |
|
until inferior mesenteric artery anterior instead of medial |
| vert location of IMA |
| L3 |
| vert location of SMA, |
| L1 |
| vert location of celiac trunk |
| T12 |
| vert location of aortic bifurcation |
| L4 |
|
suprarenel/adrenal glands -shape of left and right surrounded by? how regulate stress response blood supply? |
|
left: crescent right: pyramidal perirenal fat regulate by synthesis of catecholamines BS: superior suprarenal middle suprarenal inferior suprarenal |
|
suprarenal arteries superior middle inferior all from where? venous drainage into what? |
|
superior: inf. phrenic middle: AA inferior: renal artery suprarenal vein |
|
Where does aorta pass behind diaphragm? (aortic hiatus) where aorta pops out of diaphragm |
| T12 |
|
arteries of posterior wall (5) locations from where? |
|
inferior phrenic (A) (T12) middle suprarenal (A) (L1) renal arteries (L1) (opposite SMA) testicular/overian (A) (L2) Common iliac (L4/5) |
| inferior phrenic supplies what? |
|
inferior diaphragm, adrenal glands |
|
IVC what side of aorta enters diaphragm at what vert lvl |
|
right of aorta IVC hiatus at T8 |
| largest vein in body? |
| inferior vena cava |
| does IVC have valves? |
| NO |
| common iliac veins converge to form IVC at what vert lvl |
| L4/L5 |
|
Right side veins drain to what vein? Left side veins drain where? |
|
Right to IVC Left to Renal V |
| what runs between aorta and SMA? |
| pancreas, left renal artery, 3rd part of duodenum |
|
issue that could arise with Left renal vein running under SMA? other name forSMA |
|
anatomical nutcracker SMA gets pulled down by weight of intestines. could compress vein leading to varicoele in LEFT testicle. testicular/ovarian vein drains into left renal vein |
| why is left testicle more prone to varicoele than right? |
|
right testicular v drains straight to IVC left testicular v drains to L renal vein |
| what forms superior border of abdominal cavity? |
| diaphragm |
| diaphragm innervated what what two nerves? |
|
phrenic lower thoracic |
|
phrenic nerve responsible for what in diaphragm what else does phrenic innervate?? |
|
motor and sensory The PPPs (phram) pericardium, pleura, peritoneal cavity |
| lower thoracic nerve resposnsible for what in diaphragm? |
| sensory to periphery |
| damage of either side of phrenic n. results in what? |
| HEMIDIAPHRAGM - paralysis of a side of diaphragm |
| three parts of skeletal muscle of diaphragm |
|
vertebral/lumber costal sternal |
| Diaphragm vertebral skeletal muscle. attach where? by what? |
| L1-L3, by crura |
|
Diaphragm skeletal costal muscle form what attaches where? |
|
form the domes attach to ribs 6-12 |
|
diaphragm skeletal sternal muscle attaches where? |
| post xiphoid |
|
what joins aorta in aortic hiatus where again? |
| T12. azygos, thoracic duct |
| I eight 10 Eggs At 12, where the structures pop out of diaphragm |
|
IVC T8 Esophagus T10 Aorta T12 |
|
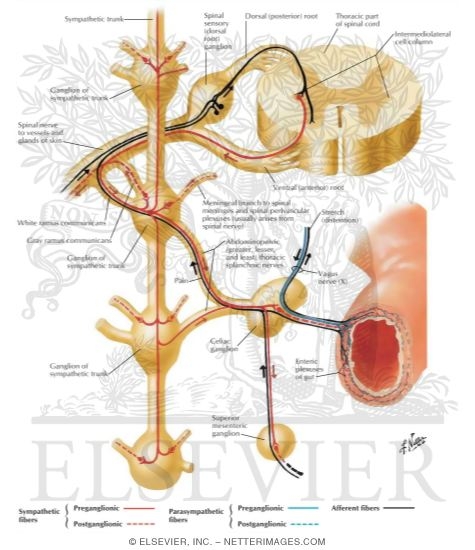
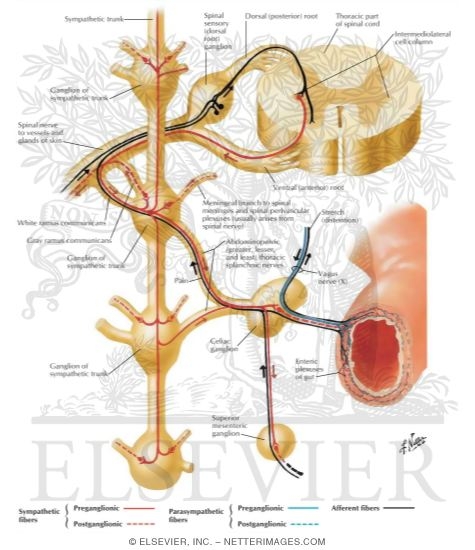
Afferent nerves -also called? -do what -where are cell bodies |
|
sensory neurons carry impluses TOWARDS CNS dorsal root ganglia Afferent Arives Efferent Exits |
|
Efferent neurons -also called? -do what -where are cell bodies |
|
motor neurons carry signal AWAY from CNS grey matter of spinal cord |
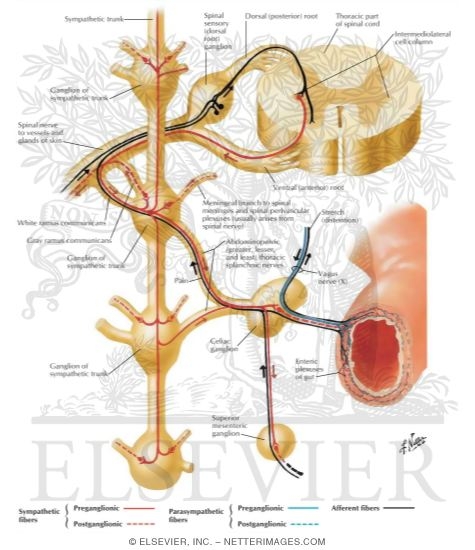
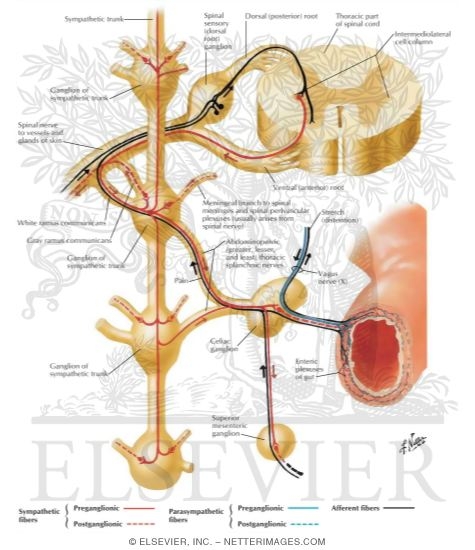
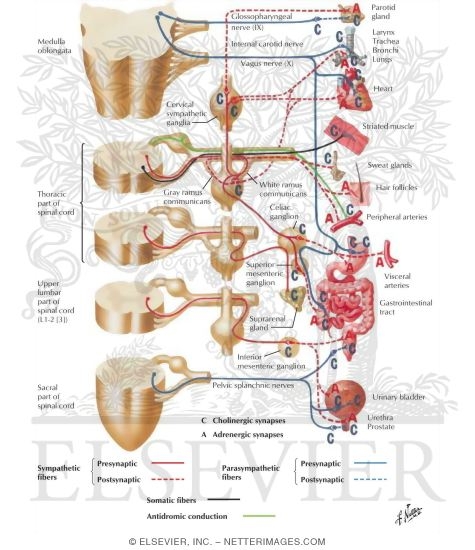
| three paths of sympathetic efferent nerves... |
|
preganglionic fibers exit ventral root, go through white rami into sympathetic trunk. Then.. 1. synapse at same level with postganglionic neuron and exit thorugh grey rami and then posterior or anterior rami to target 2. synapse at different level though grey rami, then anti or post rami, to target 3. dont synapse with splanchnic n, and go synapse at a prevertebral ganglia ( a ganglion between sympathetic trunk and organ) |
|
preverterbral gangion what? examples |
|
ganglion located between the sympathetic trunk and an organ. celiac ganglia, superior mesenteric ganglia, inferior mesenteric ganglia |
|
SAME DAVE paths of somatic afferent/efferents |
|
sensory afferent motor efferent dorsal afferent ventral efferent |
| summary of somatic nerve function |
|
impulse carried by afferent neuron (sensory) -> dorsal root -> posterior horn -> interneuron -> efferent cell body in anterior (lateral) horn -> ventral root -> body
somatic efferent/afferent 1,2
|
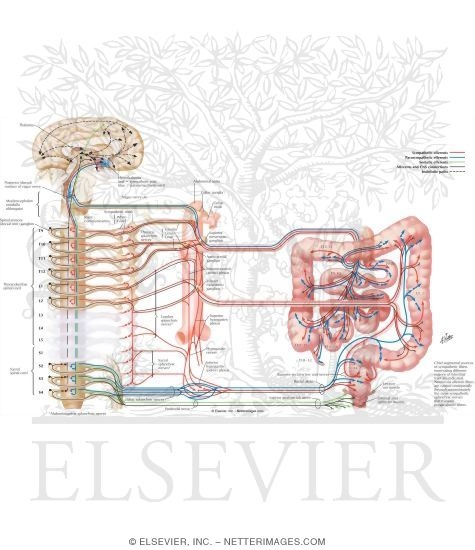
| sympathetic summary |
|
sensory impluse -> dorsal root -> spinal cord -> cell body of preganglionic neuron -> ventral root -> white rami -> sympathetic ganglion then, if heads straight to organ sympathetic ganglion -> gray rami -> anterior/posterior rami -> body
sympathetic efferent 3,4,5
|
| preganglionic cell bodies in lateral horns of spinal cord between what and what vert locations? |
| T1-L2 |
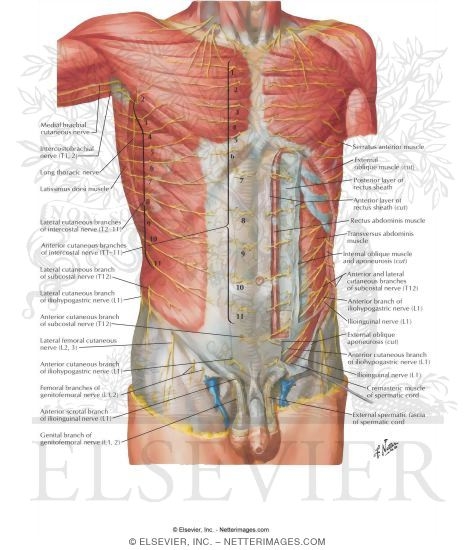
| somatic nerves to abdominal wall |
|
Phrenic (C3-5) -diaphragm Lower thoracic nerves (T7-12) intercostal nerves, rectus abdominus Subcostal nerve (anti rami of T12) EO and skin of anterolateral abd wall - not lumbar plexus nerve *palpate 12 rib to find |
| cutaneous branches of lower thoracic nerves |
|
CB around Xiphoid (T7) CB around umbilicus (T10) CB just above pubic bone T12 CB just above inguinal region (L1)
|
| sympathetic nerves/ structures |
| sympathetic trunk, greater/lesser/least splancnic |
|
parasympathetic nerves origin of pre-parasympathetic neurons? |
|
cranio-sacral: cranial derived, come off spinal cord in sacral region
vagus CNX, pelvic splancnic (S2-S4) |
| lumbar plexus |

|
| lumbar plexus |

|
|
iliohypgastric ilioinguinal
vert location? location? finish where? |
|
both L1, cross quadratus lumborum. iliohypogastric superior to ilioinguinal end up as superficial nerves on abdominal wall |
|
genitofemoral vert location? location what reflex a part of? |
|
L1-L2 on top of Psoas muscle
both sensory/motor components
femoral part -> cutaneous over femoral triangle genito part -> innervs cretmaster muscle
*part of cremaster reflex |
|
lateral femoral cutaneous location, end point? associated syndrome?
|
|
crosses across illiacus muscle, under inguinal ligament, ends on anterior lateral part of thigh (sensory)
myalgia parenthetica -tight, low pants compress nerve causing parestheia over lateral anterior thigh |
|
femoral nerve vet location? location? |
|
L2-L4 between illiacus and psoas muscles |
|
Obturator vert location? location |
|
L2-L4 medial to psoas |
|
lumbosacral trunk (lumbar plexus) vert location
|
|
L4-L5 from spinal hole to pelvis connects lumbar plexus to sacral plexus |
|
sympathetic thoracolumbar region what (nerves)? what through what? includes what chains? |
|
where preganglionic ganglia reside. T1-L2 sympathetic, thoracic splanchnic, lumbar splanchnic |
|
autonomic aortic plexus what means?
|
|
sympathetic/parasympathetic neurons running in it ganglia = postganglionic sympathetic masses
|
|
celiac plexus components also called |
|
2 celiac ganglia, 1 superior mesenteric ganglion solar plexus |
|
greater splanchnic nerves path |
|
from posterior thorax, through diaphragm greater splan = preganglionic symathetic nerve heading to synpase at post ganglionic sympathetic neurons at celiac ganglion |
|
lesser/least splanchnic nerves path |
| pierces diaphragm, go to other ganglia |
| lumbar sympathetic chain |
|
nerves coming off are pre-gangilionic sympathetic looking for post ganglionic neurons to synapse with
*post ganglionic nerves are those that actually cause reponses. |
|
|
intermediallateral cell column: where sympathetics cell bodies are located T1-L2
impluse from column heads to sympathetic ganglia and can do 1 of 4 things -synapse to postganglionic neuron ->grey -> spinal nerve going out(venral primary ramus, in this case) to some muscle/organ
-move to superior ganglion in chain - move to ganglion below -synapase with postganglionic neuron in sympathetic gangion and move out into abdomen -look for a more peripheral post ganglionic sympathetic neuron (eg. greater splanchnic to celiac ganglion) then to a target tissue by way of blood vessel
|
| what are post ganglionic fibers doing in a somatic nerve (ventral rami)? |
|
use somatic nerves to get to where they wanna go -control sweat, erector pilli muscles, smooth muscles - all sympathetically controlled |
|
|
blue structure = vagus nerve
preganglionic goes though plexus, does NOT synapse and goes straight to target tissue. post ganglionic neurons inside the target tissue itself (parasympaetheic) post ganglionic parasympathetic fibers are very short, preganglionic fibers are very long |
|
LENGTH pre ganglionic sympathetic fibers post ganglionic sympathetic fibers |
|
pre: short post: long
post are long becuase they dont lie in target tissue but in ganglionic masses |
| what kinds of neurons run along SMA? |
|
sympathetic parasympathetic sensory |
| what kinds of neurons run along IMA? |
| sympathetic and sensory |
| vagus nerve travels down what blood vessel? |
| SMA |
| how much of gut is innervated by vagus parasympatheic fibers? |
|
about 2/3rds of the transverse colon
|
|
how does the rest of gut get innervated by parasympathetic neurons if vagus only goes 2/3rd of way down transverse colon?
|
|
pelvic splanchnic n S2,3,4 keeps penis off the floo
|
|
how does pelvic splanchnic run innervations along gut?
|
|
uses superior rectal artery to ascend then spreads to hind gut using other blood vessels of IMA, but not IMA itself
|
|
general function of autonomic in GI track?
sympathetic parasym |
|
sympathetic: vaso constrictive of gut vessels parasymp: gland secretion (muscous/digestive juices), peristalsis - digestive processes |
|
visceral afferents where are cell bodies |
|
what provides sensory information to pareital peritoneum? where would cell bodies be? |
|
somatic nerves: lower thoracic (CB at xiphoid T7, CB at umbilicus T10) upper lumbar (CB atpubic bone T12, CB at inguinal region L1)
dorsal root ganglia |
|
visceral afferents
where are cell bodies?
involve what kind of receptors? |
|
like somatic afferents, have cell bodies in dorsal root ganglia
stretch (visceral stretch) receptors felt as referred pain, according to spinal cord level of sensory cell bodies)
|
|
| green: incomign afferent somatic sensory fibers, with cell bodies in dorsal root, |
|
|
visceral afferents (black)
comign from gut (eg. distended), through sympathetic ganglia -> white rami >spinal nerve >bodies in DRoot then do other stuff.
somatic/visceral afferents both enter at same place, through same root - REFERRED pain with afferents. |
| comparison of neurons |

|
|
|
referred pain (due to stretch, distention, ischemia) Hollow tube organs where is pain referred for: forgut (stomache - mid DD) midgut (mid DD to 2/3 Tcolon) hindgut kind of pain?
solid organs? |
|
along midline forgut superior to umbilicus, midgut at umbilicus hind at lower abdomen dull achey pain
solid organs usually will have pain over the organ itself |
|
when will visceral referred pain become localized?
|
| when the organ irritates the parietal peritoneum (somatic) |
|
visceral pain is:
somatic pain is:
both can abe referred |
|
dull, achy poorly localized
the opposite
|
| lymph drainage of testes/scrot/abdomen |
|
lymph usually follows vessels.
|
|
cisterna chyli what? where? gets lymph from where |
|
bag right behind diaphragm where aorta comes in. receives lymph from lower parts of body and drains to thoracic duct
form aortic lymphatic areas preaorta - lie on top of aorta, drain intestines (particularly unpair arteries) para-aortic/lumbar - drain deeper structures; two chains
from feet up
para aortic -> pre aortic - cisterna chyli - thoracic duct |
| lymph from testes |
|
development in abdominal cavity, lymph vessels and blood vessels form up there
different from kidney which looses/reestablishes blood supply as develops, the testes pull their blood supply down with them AND LYMPH DRAINAGE
so lymph goes up testicular vessels and wind up in lumbar/para-aortic lymph nodes then across intestinal nodes to cisternal chyli |
| lymph from scrotum |
|
scrotum is an outpocketing of anterior abdominal wall
lymph first to inguinal nodes (superficial inguinal nodes) then to deep ones > follow iliac vessels and end in lumbar/para aortic nodes |
|
when do major organ systems form in the embryo? what is important about this period? |
|
4-10 weeks, embryonic period. also time in which embryo most susceptible to outside influences |
|
primitive gut from what embryonic layer? into how many layers does it branch, names? how is it suspended? |
|
endoderm, tube in a tube. 3 segments: foregut: esophago - mid duodenum midgut: mid duodenum - 2/3 Tcolon hindgut: 1/3 Tcolon to 1/2 anus suspended by ventral/dorsal mesentary |
|
Weeks 6-9 what major thing happens (digestive) what main misformations could happen? |
|
hollow primitive tube forms from folding/enlongating of embryo. if endoderm fails to properly recanalize: stenosis, atresia, duplication |
|
esophageal atresia what? |
| causes esophagus to end as a blind pouch. will usually attach to trachea distally |
| what nerve flanks developing stomach? |
| vagus |
| in formation of stomach curves, why is one bigger than other? |
| greater curvature resulted from the dorsal wall of stomach growing faster then the ventral wall. at this point in embryo, "greater curve" was posterior and "lesser curve" anterior |
| after curves of stomach established what happens? |
|
stomach rotates 90 degrees clockwise, forming a lesser sac (OMENTAL BURSA) posterior now greater curve/dorsal side facing left |
| after rotation what is orientation of vagus nerves? |
|
left become anterior, right posterior originally on right and left sides of hollow tube, tube distends dorsally then rotates. nerves left on their side of thinner tube just anterior and posterior |
| which vagus nerve is anterior? |
| LEFT |
| so, distenstion, rotation then what? |
|
stomach pushed up, moving clockwise when taking a lateral view from left side (dorsal ventral axis) and given a backwards C shape post natal orientation of duodenum /stomach attained dorsal mesentary gets stretched as stomach moves forming greater omentum ventral mesentary attached to developing liver now the lesser omentum |
| greater omentum forms from what side of growing mesentary? |
| dorsal |
|
during stomach rotating/bending what is prone to atresia/stenosis? artresia in this case mean? major cause of stenosis |
|
pyloric canal/sphincter part of duodenum has no lumen and shut tight. hypertrophy of muscles in pyloric region |
| what is epiploic foramen very close to |
| hilum of liver |
|
formation of midgut begins as? what happens next: |
|
primary intestinal loop due to lack of space, midgut gets forced to herniate through umbilicus into umbilical cord as it does this it undergoes 90 degree counterclockwise rotation (looks like string twisted) around SMA (chillin in body but attached via branches) |
|
during week 10 when more space is made available in body cavity how does midgut get incorportated back into body? which first, cecum, Tcolon, intestines? TCOLOn in relation to SMA |
|
180 degree counterclockwise rotation and RETRACTION cecal bud acts as knot on rope and stays in umbilicus, allowing intestines to go first which go and get settled on the LEFT, then Tcolon then cecum SMA posterior to Tcolon |
|
what happens once intestines are back in cavity? last step in this development? |
|
ascending colon elongates and pushes cecum/appendix down inferiorly to it's usual spot ascending/descending colon's mesentaries fuse with posterior wall to become secondary retroperitoneal VIA MESOCOLON |
|
difference betweet: LIGAMENT MESO - (SOMETHING) OMENTUM |
|
LIGAMENT = no vessels MESO = has vessels OMENTUM = attaches organs |
|
Omphalocele what? how corrected? |
|
when abdominal cavity too small is doesnt permit return of instestines from umbilicus. place elastic tube over the omphalocele and gradually twist organs into place |
|
Meckle's diverticulum 2s!!!!!! |
|
portion of yolk stalk that doesnt degenerate. hangs of ilieum. -can become inflammed -attached to umbilicus by a ligament. - this ligament may be PATENT, some poop comes out umbilicus 2 in long, 2 ft from ileocecal junt, 2x more in males, 2% of pop |
|
left sided colon results from? |
| failure of 180 degree rotation when returns to cavity. Large intestine on LEFT, small instestine on RIGHT |
|
reversed rotation caused by? what enters cavity first? tcolon in relation to SMA problem that could encounter? |
|
when rotating 180 before coming back in cavity, intestines rotate clockwise instead of counterclockwise. cecum/Tcolon enter first SMA anterior to tcolon -tcolon could get compressed by SMA/pinned under duodenem when attaches to posterior wall tcolon could get |
|
in normal development where is Tcolon, duodenum, small instestine, sma? |
| duodenum/small intestine posterior to Tcolon. SMA posterior to Tcolon |
|
subheptaic/fetal cecum what is? when becomes a problem? |
|
ascending colon doesnt elongate and cecum remains undescended. problem when appendicitis happens, mistaken for cholecystisis |
|
point fixation with volvulus what is? |
|
portion of intestine gets fixed to body wall while other portions are still mobile. twist upon themselves = volvulus twisted portion can become ischemic |
| % people with malformed midgut |
| .2% |
|
situs inversus what? results in? |
|
reversal of all body organs! left sided appendix |
| formation of diaphragm what 4 structures must fuse? |
|
pleuroperitoneal mem mesentary of esophagus thoracic wall covering septum transversum
|
|
septum transversum (part of diaphram formation) ends up becoming whaat of diaphram? forms into what outside diaphragm? |
|
in diaphragm: central tendon (attaches to xiphoid) houses the hiatus of IVC
outside diaphram: ventral mesentary of foregut (becomes lesser omentum) |

|
|
IVC in central tendon esophageal hiatus aortic hiatus (formed byt cruras) |
| by what week is diaphram innervated by phrenic n? |
| 4 |
| diaphragm descends to L1 by what week? |
| 8 |
| malformations when structures do not fuse correctly to form diaphragm: |
|
foramen of morgagni Pleuroperitoneal mem abscense esophageal hiatus foramen of bochdalek |
| esophageal hiatus hernia |
| caused by loose connection between esophagus/diaphragm which allows esophag/stomach to slip upwards - pushing esophageal sphincter upwards |
|
foramen of morgagni (hernia /sternal slip) foramen of bochdalek (lumbocostal trigone)
|
|
morgagni: hernia close to sternum (anterior) bochdalek: hernia at lumbar/costal trigone (poserior) |
| pancreas development |
|
develops from two buds: dorsal and ventral (from liver bud)
grow more dorsal than ventral. dorsal then rotates towards posteriorly to join dorsal bud.
|